The Primary Care Behavioral Health Integration Program is currently offered at select Children’s Primary Care Medical Group and Children’s Physicians Medical Group locations. It is designed to improve the emotional well-being of children and adolescents through conducting early identification screenings, increasing access to behavioral health care, implementing prevention programs and providing evidence-based treatment. This is accomplished through having an integrated health therapist embedded in the primary care office.
Benefits of Primary Care Integration
- Convenient in a setting that is familiar and more comfortable for the child
- Unified team that provides patients with more consistent care, centered around the pediatrician
- Same-day access to an IHT, typically a licensed clinical social worker, marriage and family therapist, professional clinical counselor or psychologist
- Evidence-based approach with consistent protocols
- Medical and mental health services provided together seamlessly at the same location with structured referrals and interdependent consultations
- Family-centered, collaborative approach
- Mental health screenings, assessments and registries
- Psychiatrist case consultation
- One integrated treatment care plan with both behavioral and medical components, including shared electronic health record and IT tools
- Enhanced knowledge of pediatricians about how behavioral conditions impact medical treatment (and vice versa)
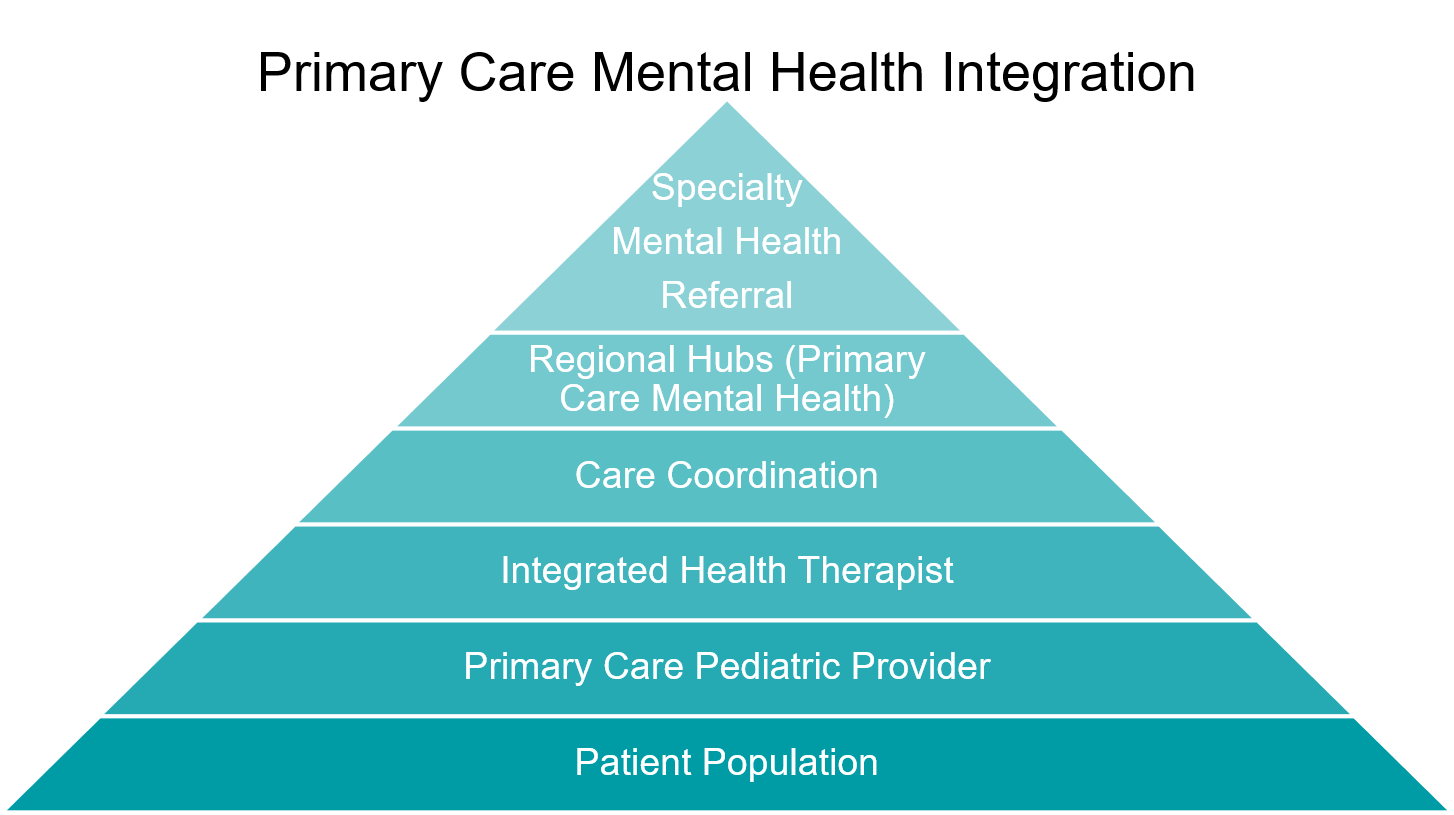
The pyramid below shows the layers of primary care integration and how PCMHI fits into the broader patient care continuum.
Need for Primary Care Integration
Up to 90 percent of people who receive treatment for a behavioral health issue recover. However, one of the largest barriers to treatment is lack of access to care.
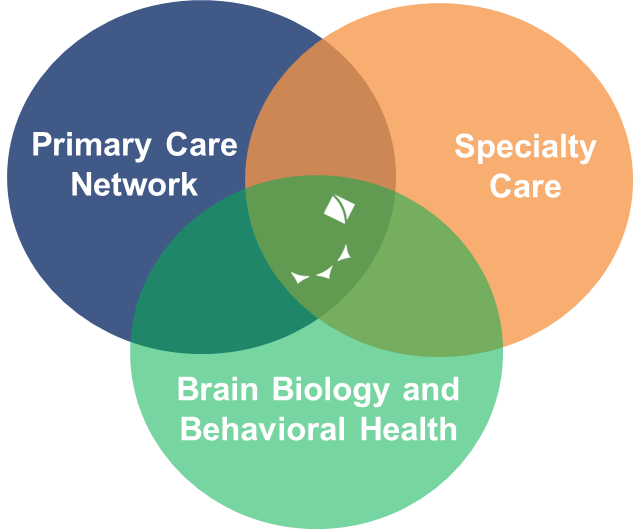
Mental health services have historically experienced a divide between physical healthcare, access, delivery and reimbursement. Through PCMHI, we are bridging these gaps, providing enhanced care coordination through evidence-based protocols. IHTs are available to meet briefly, where feasible, on the same day as the child’s pediatrician appointment,* and then provide short-term, ongoing therapy in the same office for seamless integration of behavioral and medical care.
*Select locations
Primary Care Integration Network
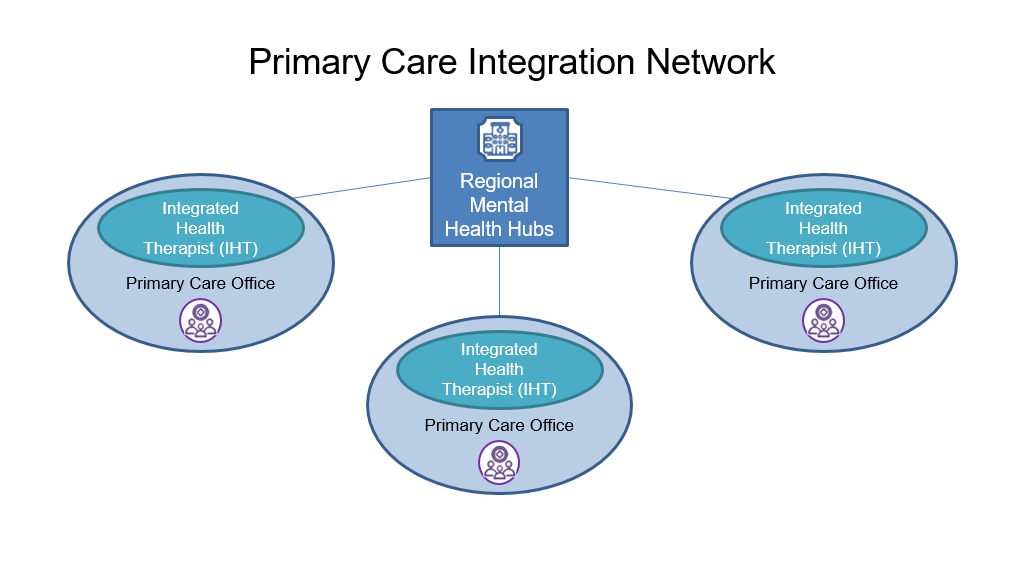
PCMHI addresses lack of access to mental health care through early identification and rapid connection to “Primary Care Mental Health” through a hub and spoke model. Patients are identified in the primary care setting and referred to the regional hub as needed.
- Primary Care Sites are embedded with an IHT to streamline mental health services alongside medical care. IHT offices are located in the same office as the PCP. They provide shorter treatment plan lengths per patient.
- Regional Mental Health Hubs are referral places for more advanced cases of mental health diagnosis. They provide longer term treatment plans, as well as more extensive levels of mental and behavioral care.
Evidence-Based Model
Below are evidence-based research articles that build the case for the effectiveness of primary care integration.
- Hall, J., Cohen, D. J., Davis, M., Gunn, R., Blount, A., Pollack, D. A., … & Miller, B. F. (2015). Preparing the workforce for behavioral health and primary care integration. The Journal of the American Board of Family Medicine, 28 (Supplement 1), S41-S51.
- Cohen, D. J., Balasubramanian, B. A., Davis, M., Hall, J., Gunn, R., Stange, K. C., … & Miller, B. F. (2015). Understanding care integration from the ground up: five organizing constructs that shape integrated practices. The Journal of the American Board of Family Medicine, 28(Supplement 1), S7-S20.
- Collins, C., Hewson, D. L., Munger, R., & Wade, T. (2010). Evolving models of behavioral health integration in primary care. New York: Milbank Memorial Fund, 504.
- Butler, M., Kane, R. L., McAlpine, D., Kathol, R. G., Fu, S. S., Hagedorn, H., & Wilt, T. J. (2008). Integration of mental health/substance abuse and primary care. Database of abstracts of reviews of effects (DARE): quality-assessed reviews [Internet].
- Asarnow, J. R., Rozenman, M., Wiblin, J., & Zeltzer, L. (2015). Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: a meta-analysis. JAMA pediatrics, 169(10), 929-937.