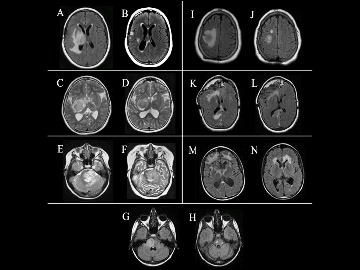
Serial T2-weighted axial magnetic resonance imaging findings in seven patients before and after HBOT. A: Patient #1 eight months after radiation therapy demonstrating edema extending around resection cavity, and B: after HBOT showing decreased edema. C: Patient #2 showing enhancing mass in right medial temporal lobe, basal ganglia, and D: after HBOT grossly unchanged. E: Patient #3 with malignant transformation of previously low-grade glioma four months after radiation therapy, with large peripherally enhancing mass in pons, and F: after HBOT demonstrating interval progression and enlargement of mass. G: Patient #4 11 years after radiation therapy with right pontine mass, biopsy-proven radiation necrosis, and H: after HBOT showing decreased size of pontine lesion. I: Patient #5 nine months after radiation therapy, with residual tumor in right parietal lobe along with radiation necrosis, and J: after HBOT with marked improvement in edema. Patient also had PET imaging with no abnormal FDG uptake, suggesting radiation necrosis. K: Patient #6 four months after radiation therapy with areas of T2 prolongation likely post-radiation changes and known deformity of anterior cranial vault consistent with history of fibrous dysplasia and post-operative changes, and L: after HBOT with decreased T2 signal abnormalities M: Patient #7 six months after radiation therapy demonstrating abnormal signal within bifrontal peri-ventricular white matter and adjacent to frontal horns, and N: after HBOT with improvement of periventricular abnormalities but with progressive disease in frontal lobes.
A recently published study by John Crawford, M.D., M.S., and researchers at Rady Children’s and UC San Diego finds hyperbaric oxygen therapy (HBOT) to be safe and efficacious in pediatric and young adult patients with central nervous system (CNS) tumors.
HBOT is the use of oxygen at elevated atmospheric pressure. It has been well-established for treating a variety of conditions, including gas embolism, carbon monoxide poisoning, decompression sickness, radiation cystitis, radiation proctitis and delayed wound healing. The therapy allows increased oxygen delivery to tissue via hemoglobinin-dependent transport and is thought to reduce inflammation and lead to neovascularization of irradiated tissue.
HBOT has also been studied for adjunctive therapy in the treatment of brain tumors. As an adjunctive treatment with radiotherapy or to treat CNS radiation necrosis (RN), HBOT has shown promise in a few case series, and to date no randomized controlled trials have been conducted. The safety and efficacy of HBOT in pediatric patients is less understood.
In the current study, the researchers performed a retrospective analysis of their single institutional series of pediatric and young adult brain tumor patients who underwent HBOT. Seven patients (ages 10-23 years, six females) were treated with HBOT (three-60 sessions) for either RN (n = 5) or tumor-associated edema (n = 2). Tumor diagnosis included low-grade glioma (n = 4, two with neurofibromatosis type 1), meningioma (n = 1), medulloblastoma (n = 1) and secondary high-grade glioma (n = 1). Prior therapies included surgery (n = 4), chemotherapy (n = 4) and radiation (n = 5: four focal, one craniospinal). Three underwent biopsy: one confirming RN, one high-grade glioma and one low-grade glioma. Patients were assessed for clinical and radiographic changes post HBOT.
The median time to clinical and radiographic presentation was eight and a half months (range six months–11 years) in those who had prior radiation. Clinical improvement after HBOT (median: 40 sessions) was observed in four of seven patients. Symptoms were stable in two and worsened in one patient. Radiographic improvement was seen in four patients; three had radiographic disease progression. In the subgroup treated for presumed and biopsy-confirmed RN (n = 5), four of five (80%) had clinical and radiographic improvement. There were no long-term adverse events due to HBOT.
Based on these results, the researchers concluded that HBOT appears safe and well-tolerated in pediatric and young adult brain tumors. HBOT was shown to be most effective for patients with biopsy-confirmed or presumed RN.
Dr. Crawford says that future clinical trials are planned to explore the possibility of HBOT as an adjunct therapy in the treatment of childhood brain tumors with our without radiation therapy. “Alternative therapies to high-dose steroids are much needed given the degree of side effects our patients experience,” he notes.
“Use of hyperbaric oxygen therapy in pediatric neuro-oncology: a single institutional experience” was published online in the Journal of Neuro-Oncology on Nov. 13, 2018.