Congenital Diaphragmatic Hernia Overview
Rady Children’s Comprehensive Congenital Diaphragmatic Hernia (CDH) Center, which is part of our
top-ranked Neonatology program, is dedicated to providing the most advanced care for infants and children with this type of birth defect. Our multidisciplinary approach from a highly skilled team of specialists enables your child to receive the best possible treatment.
During this challenging time or a baby’s CDH, health professionals will be with you every step of the way, providing family-centered, compassionate and personalized CDH care.
Infants and children treated at Rady Children’s Hospital have a survival rate exceeding the national average, with a greater than 95% survival for the last three years.
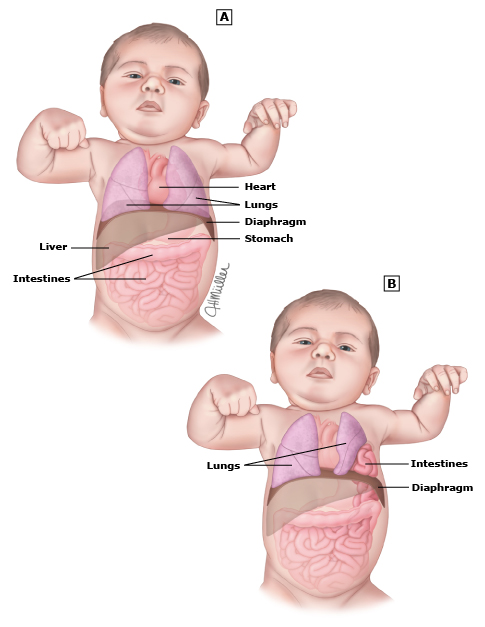
 Infants born with congenital diaphragmatic hernia have a hole in the diaphragm, allowing abdominal contents to migrate up to the chest. This leads to underdevelopment of the lung and difficulty breathing after birth. Depending on the severity of the birth defect, including issues with abdominal organs and underdeveloped lungs, a baby’s CDH can be life threatening.
Infants born with congenital diaphragmatic hernia have a hole in the diaphragm, allowing abdominal contents to migrate up to the chest. This leads to underdevelopment of the lung and difficulty breathing after birth. Depending on the severity of the birth defect, including issues with abdominal organs and underdeveloped lungs, a baby’s CDH can be life threatening.
At our CDH center, your child will be seen by experts in their fields throughout their journey. If your baby’s condition is diagnosed prenatally, you will be seen in our Fetal Care Program by a specially trained pediatric surgeon and neonatologist to discuss the diagnosis and what to expect especially if your baby has severe CDH. After delivery, your baby will be transferred to the Rady Children’s NICU.

Grace Holbrook spent her first 90 days in the NICU at Rady Children’s Hospital due to being diagnosed with a congenital diaphragmatic hernia and congenital heart disease. Now, the 5-year-old is happy, healthy and a part of the Rady Children’s family. Meet Grace.
In the NICU, your baby will receive treatment to help them breathe and protect their lungs. For CDH patients who fail to respond to standard or innovative therapies, we offer extracorporeal membrane oxygenation (ECMO) a form of life support used for patients with life-threatening heart and/or lung problems. Should ECMO become necessary because of severe CDH, we have a dedicated team of ECMO providers at Rady Children’s Hospital to treat your child.
The medical and surgical teams work closely to determine the optimal timing of the surgical repair for CDH patients. After your child recovers, CDH care will shift to include the developmental skills of your baby under the supervision of our physical therapists and occupational therapists.
After you leave the hospital, your baby will be seen by our renowned Pediatric Surgery program and the NICU Neurodevelopmental Clinic to focus on developmental care. Based on the individual needs of the infant at the pediatric surgery program, follow-up care for the baby’s conditon may also be scheduled with Pulmonary/Respiratory Medicine, the Pulmonary Hypertension Program, Gastroenterology, Hepatology & Nutrition, Occupational Therapy, Physical Therapy and the Dysphagia team.
Learn more about CDH and what to expect.
Why Choose Rady Children’s?
- 24/7 care by our attending neonatologists and pediatric surgeons to address all of your child’s medical needs (consistently top 10 rated neonatology program in the nation by U.S. News & World Report)
- ELSO Center of Excellence (designated by Extracorporeal Life Support Organization) which highlights our commitment to quality, patients and families
- Access to cutting-edge ultra-rapid genomic sequencing at Rady Children’s Institute for Genomic Medicine
- Prenatal diagnosis
- Fetal magnetic resonance imaging (MRI) to evaluate CDH severity
- Support by nationally ranked heart and heart surgery programs
- Ongoing care coordination
- Advanced research by physician-scientists
- Highly trained family support team of physicians, social workers and therapists
- Chaplain support
About CDH: What is a Congenital Diaphragmatic Hernia and How Does It Affect Babies?
Congenital diaphragmatic hernia, or CDH, is a birth defect in which the diaphragm has a hole that allows organs from the abdomen to push up into the chest. During the baby’s development, a portion or all of the diaphragm on one side fails to form, creating the hole. Abdominal contents in the chest prevent lung growth on the affected side. With CDH in babies, the airways and blood vessels of the lungs also develop abnormally.
What Are the Types of Diaphragmatic Hernias?
Diaphragmatic hernias can be broadly classified into two types:
- Congenital Diaphragmatic Hernia (CDH)
- Acquired Diaphragmatic Hernia
The first signs of diaphragmatic hernias in babies may include difficulty breathing, rapid breathing, abdominal distension shortly after birth, bluish discoloration of the skin (cyanosis), as well as pulmonary hypertension which is a condition that makes it difficult for blood to circulate through the underdeveloped lungs.
If diaphragmatic hernia is suspected, immediate medical attention is necessary, and your child should be tested and diagnosed as soon as possible after birth or even during a prenatal ultrasound in some cases.
What Diagnosis Procedures Are Used to Determine the Types of Diaphragmatic Hernias?
CDH is typically identified by fetal ultrasound. When detected prenatally you will be referred to a perinatologist, a pediatric surgeon and a neonatologist to discuss what type of CDH your baby has and what to expect. Your baby will be followed by ultrasound. A fetal echocardiogram will be performed to evaluate the structure of the heart. A magnetic resonance imaging exam will also be arranged. Your baby’s delivery will be planned at a tertiary medical center with direct transfer to Rady Children’s Comprehensive Congenital Diaphragmatic Hernia Center.
The type of babies affected the most by diaphragmatic hernias are infants who are born with this defect. CDH occurs in approximately 1 of every 3,000 pregnancies. Sometimes CDH is diagnosed after the baby is born. If a diagnosis is made your baby is born, you and your baby will be transferred directly to Rady Children’s Hospital.
Treatment for Diaphragmatic Hernias
Most babies with CDH will need a breathing tube and may need help from a ventilator for many weeks. Your baby will be seen by a neonatologist and a pediatric surgeon. Consults to other specialties including genetics, cardiology, pulmonary hypertension, pulmonology, and gastroenterology will occur as needed.
Complications from types of diaphragmatic hernias include respiratory distress and underdeveloped lungs. Babies with CDH can have other problems outside of lung growth issues. Your baby will have imaging of their brain, heart and kidneys.
Once your baby is fit for surgery, our healthcare professionals will then repair the hole in the diaphragm and replace the intestines and other organs back in the abdomen. The timing of repair will be carefully decided based on your baby’s individual case.
An umbilical venous catheter or a peripherally inserted central catheter will be placed for health professionals to give IV (intravenous) medications, including blood pressure medications and IV nutrition. An umbilical arterial catheter or a peripheral arterial line will be placed to accurately measure blood pressure and for frequent lab draws.
ECMO (extracorporeal membrane oxygenation), therapy may also be recommended which is a heart-lung bypass treatment that can allow time for pulmonary hypertension to improve. Other treatments include inhaled nitric oxide and Heliox, an inhaled helium-oxygen mixture that improves the removal of carbon dioxide and eases the work of breathing.
What Happens After CDH Patients Have Surgery?
After the CDH has been repaired, respiratory support will gradually be weaned. When your baby no longer needs assistance from the ventilator, the breathing tube will be removed. Your baby may temporarily need CPAP (continuous positive airway pressure) or a nasal cannula to make his/her breathing easier. In some cases, babies need to go home with oxygen after seeing healthcare providers.
Babies with CDH cannot be fed until after the hernia is repaired by healthcare professionals. Your baby will receive full IV nutrition from TPN (total parenteral nutrition) while awaiting surgery. After surgery, your baby will be monitored for feeding readiness. Babies may require careful dietary restrictions during their recovery period. Your baby will be followed by an occupational therapist, lactation consultant and registered dietician to support feeding and nutrition.
The length of your hospital stay will vary depending on the severity of your baby’s CDH.
Follow-up Care
For babies with CDH, a pediatrician is needed to coordinate care from multiple specialists. At Rady Children’s Hospital, we take a multidisciplinary approach to provide your child with advanced care from a highly skilled team of healthcare professionals, ensuring that babies receive the best possible treatment and personalized care.
After you leave the hospital, your baby will be seen by health professionals in our Pediatric Surgery program and the NICU Neurodevelopmental Clinic to focus on developmental care. Babies with CDH may continue to have medical issues after leaving the hospital. Your baby may also require a referral to the Rady Children’s Pulmonary Hypertension Program to be seen by a cardiologist and pulmonologist.
Contact Our Staff for CDH Prenatal Diagnosis, Treatment, and Surgery
If you need assistance with diagnosis, treatment, or surgery for CDH, you can contact Rady Children’s Hospital Fetal Care Program Coordinator at:
Phone: 858-966-5475
Email: fetalcareprogram@rchsd.org
